Sure you must be super fit?
Are you able to treat yourself?
You must never get injured?
It must be great be able to get massages every day!!
Guess what ?? Physios get injured and we here are at Physio Performance Drogheda are no different.
Sometimes we are the biggest hypocrites and we don’t always practice what we preach!!!!!
Although injuries are never nice and they are frustrating, they can be a learning experience and I am going to bring you through my own injury journey.
A Little History First
In January last year having returned from living in the UK for a few years I started back into pre-season training with my local GAA club. Training was as you’d expect for that time of year, muck up to your knees, plenty of running and a lot of lads blowing black smoke after an enjoyable winter!!
I was actually going well in terms of fitness, leading some of the hard slogging and overall, I was feeling good considering I has been away from football for the last 4/5 years. In addition, away from the pitch I had been doing a lot of my own work (I knew the ball handling wouldn’t be great so I needed all the help I could get!). So for the first 3 months I felt all was going well in terms of training and was looking forward to the season getting under way.
The Warning Signs
First few games went as you would expect a little (very) rusty but starting to get back into the swing of things. It wasn’t until April that year during a match when in the last 10 minutes I felt a soreness in my left groin. Now I have never had any groin trouble, so I simply put it down to a small niggle, nothing to worry about.
The pain actually got worse after the game and was sore to walk, even getting into the car after the game was painful. So when I got home and put it up, I got some ice on it and got a night sleep. When I woke in the morning the pain was gone!
“Happy days” I thought to myself, it was only a groin strain. So that week I returned to training as normal but with no such luck. Following training I was getting this increased groin pain which if anything was getting worse after each session. However, in my head I told myself that I could manage it in between games and training as once I was warm I felt fine (Physios are the worst patients).
The “Stupidity” Cycle
So, after each training session or match, the next morning in the clinic I would get Mick to do some work on me, anything at all that would help in order for me to be fit to line out for the next game and this continued on for a couple of months. I was trying to continue with my strength work away from the pitch but majority of the time I was too sore to do anything so as a result all I could do was some gentle mobility work and swim. Now you don’t have to be a physio to see that the way I was “managing” my injury was ridiculous, but it was my first season back in over 4 years and the last thing I wanted to do was cry off with an injury!
So I carried in this same cycle until October until the season was finished and if the truth be told I dreaded training and games by the end of it. I was simply going through the motions, operating at 50% during training and barely able to get out of bed after games. In the clinic I couldn’t demonstrate exercises to patients as I was in too much pain. It even got to the stage where I used to dread sneezing or coughing as I would be bent in two with the pain when I was at my worst, it was horrendous.
The Injury
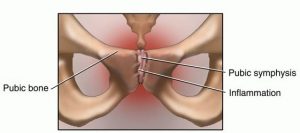
All along I knew in my head it was Osteitis Pubis or more recently known as adductor related groin pain. In technical terms. Osteitis Pubis (OP) describes a pattern of tissue damage, chronic dysfunction of the adductors (groin muscles), pubic bone and pubic symphysis caused by repetitive trauma or excessive stress across the pubic joint (Fricker et al 1991).
Patients usually experience groin pain that gradually develops over time. Symptoms worsen, with pain migrating to the pubic bone, hip flexors and sometimes lower back. Exercise such as running, kicking, changes in direction and explosive movements usually makes the pain worse. Fully developed cases may be sensitive to all weight bearing movements and even coughing or sneezing (Fricker et al 1991)
I had an MRI done which confirmed OP along with adductor gracillis dysfunction which was to be expected. It was now November and all football was finished so I now had the chance to let it settle, daily activities were all still very sore.
Active rest is the key with Osteitis Pubis. We know that by simply resting this will not bring about the changes necessary to improve symptoms. For traumatic tissue injuries like muscle or ligament tears rest and a slow return to activity is the right move. It gives your acute trauma time to heal. But OP is not an acute injury, OP is a chronic injury. It’s the accumulation of hundreds of little micro traumas caused by your poor biomechanics (Angoules et al 2015). That recovery plan will not work because it does not change your biomechanics.
“False Dawn”
So I began to do what I could rehab wise, pain dictating everything I was doing. I started with simple mat based isometric exercises before building my way up to full strength compound movements. Strength and control around the Hip complex is imperative to bring about a reduction in symptoms (Pizarri et al, 2008)
Daily activities settled down and rehab was also going well. I even went skiing for New Years and had no pain after it. “Brilliant” I thought to myself, preseason is just around the corner and I’m almost pain free. So, in my eager state I thought I’ll try some runs and see how it is before we get back pre-season training.
Disaster!!…Started to get sore after 5 minutes but in my head, I thought maybe it just needs to loosen out I’ll be fine. I was wrong!
After 15 minutes I had to stop due to the pain and following the runs I felt like I was as sore as I had ever been. I wanted to scream the place down as in my head I was back to square one.
The real road to recovery
The next morning, I had a bit of melt down and decided the best next step would be to go to see Dr Andy Franklyn Miller in Sports Surgery Clinic to get a second opinion, a specialist with regard to athletic groin pain.
Dr Miller spoke about various different treatment options in order to get on top of my groin pain. He stated that previously I would have been referred for a steroid injection to the adductor muscles or pubic bone and symphysis however recent evidence has shown that this merely masks the root of the problem (Angoules et al 2015).
Instead Dr Miller stated that I have more than likely have underlying weakness leading to poor and inefficient movement patterns. These faulty firing patterns change the way you move, causing you to overload and overuse your adductors, creating your very own OP mechanics (Hiti, Corey J., et al 2011).
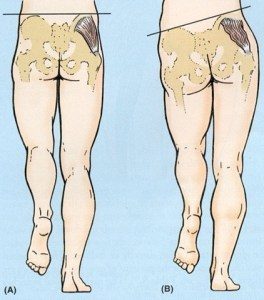
With OP there are often several different factors that need to be addressed with regard to biomechanics: increased anterior pelvic tilt, hip drop, knee valgus, over pronation/supination of the foot, poor core strength and proximal hip strength (Gore, Shane, et al 2016).
So, following a 3d biomechanics assessment it was obvious I lacked control of my left side during all single leg activities, displaying a large hip drop in landing. A hip drop occurs when poor firing patterns prevent the body from stabilizing and controlling the pelvis. You fail to maintain a neutral pelvis once the foot leaves the ground. This causes the hip to twist and rotate as the pelvis collapses towards the ground.
The shift in pelvic position also places strain on the adductors because the pubic bone drops along with the rest of the pelvis. OP patients use their adductors to help control this change in pelvic position. Shifting the pubic bone increases the tension/load on the adductors, asking them to compensate for the hip drop from a disadvantaged position.
Naturally I have an anterior pelvic tilt but when running it was clear this was becoming exaggerated and was almost dipping forward with every stride. The dipping of the pelvis also has a direct effect on the pressure/load distributed into the pubic bone. Your rectus abdominis attaches to the top of the pubic bone. As you tilt, your stomach pushes forward, stretching and straining your abdominals. This stretch increases the pull of the distal portion of your abdominals on the top of your pubic bone. In addition, your adductors attach to bottom of your pubic bone. With an anterior pelvic you now have tight adductors pulling your pubic bone down, and over stretched abdominals pulling your pubic bone up.
The Hard Work
So, it was pretty clear that I had a lot of work to do and I was given a time frame of 9 weeks before returning to play. In addition, I had several outcome measures and rehab goals that I needed to reach every two weeks which I felt really helped. With a long-term injury, it can get frustrating at times watching your teammates train away whilst you have to do rehab on your own in the gym. Small as it may seem these little targets along the way really helped to keep me on track as I now had an end goal and wasn’t just living in hope.
After 5 weeks my rehab was going well and I was hitting all the necessary targets. Daily activities were all pain free and even my general mood was improved. It was at this point I started back running which was the one element of the rehab I was worried about. Changing running mechanics can be a difficult one as unless it is a component of your training which you addressed prior to injury, it is a movement pattern which is hardwired into your brain. But as Dr Miller explained I am never going to change the way I run completely, but if I could improve 600 out of every 1000 steps I take for example this would have a positive effect on my symptoms.
Even though now I was back straight line running it was imperative that my strength and control work was as consistent as ever. Exercises such as your front squat, deadbugs, etc were all vital in avoiding that excessive anterior pelvic tilt that was previously aggravating my symptoms. Following the first few runs there was slight discomfort but nothing that I wasn’t expecting. We employed a motto which is simple but very important with regard to return to play following a long-term injury – “Never start a session sore”. So regardless of where I was in my programme or what goals needed to be reached I would give myself as much recovery as I felt necessary.
From here we continued to up the intensity of the runs whilst adding in change of direction drills with some light ball work. Progression to the multidirectional drills focused on the rate of force development across all three planes and reactive agility to prepare for sports-specific movements. No part of the rehab was rushed which I felt was important. I even took an extra week to clean up my cutting technique as following analysis I was still letting my knee fall in on the turn which was in turn causing excessive hip drop, a sure way to aggravate my old symptoms.
Load management and monitoring training is vital on returning to play following a long-term injury to avoid any spikes in capacity levels (King et al 2016). For this reason, I had to be very strict on returning to training. I done this by simply integrating back into doing the warm up and then topping up the session with my own runs. Then the next session I done 30 minutes with no high intensity cutting drills and again topping the session up with my own rehab. I continued to do this until for a further 2 weeks until finally I felt confident enough to do a full session and it felt great!
Again, the ball handling and positioning left a bit to be desired, but I didn’t mind, I could now run pain free and was back on the pitch with rest of my teammates instead of in the gym. Following the initial few sessions I was a little stiff but nothing I wasn’t expecting considering how long I had been out for.
The Reward
The following week I played my first half of a match with no repercussions. These 30 mins probably didn’t seem like much to anyone else but for me this is what I had been anticipating for almost a year, to be able to run and compete without the worry of pain or discomfort. Even the next day to be able to go to the gym and exercise pain free was a huge relief.
In the past few weeks I have been back into full training and competitive games whilst continuing to manage my load as to prevent overload and risk reinjury but overall I feel good.
What I learned
On reflection there are so many things I have learned throughout this journey:
Instead of trying to “manage” it and just get through the season I should have taken the appropriate time out before returning to play as opposed to wait until it became debilitating. Prevention is always better than cure.
Gaining an understanding of my injury along with an insight into the biomechanics of what was causing the problem was also vital in the success of my rehab.
Although an expert in my field, learning to step back slightly and let someone else guide me objectively proved crucial also.
So after the most frustrating injury of my life, it has actually developed me both personally and professionally.
If this story is similar to yours and you have been struggling with Osteitis Pubis or groin pain contact us here at Physio Performance on 041-9877059 or click here to Book Online.
Make sure to check out park two of our Osteitis Pubis blog here!